The combination of atomoxetine and dronabinol for the treatment of obstructive sleep apnea: a dose-escalating, open-label trial
- S-Med

- Sep 4, 2025
- 2 min read
The main finding of this study is that the combination of atomoxetine and dronabinol administered for 2 weeks at escalating doses may result in a reduction in OSA severity and self-reported symptoms. Increasing the dose of dronabinol beyond 5 mg does not seem to yield further clinical benefit. Although promising, a factor that could limit the potential clinical applicability of this drug combination are the several, psychotropic side effects observed after the addition of dronabinol to atomoxetine.
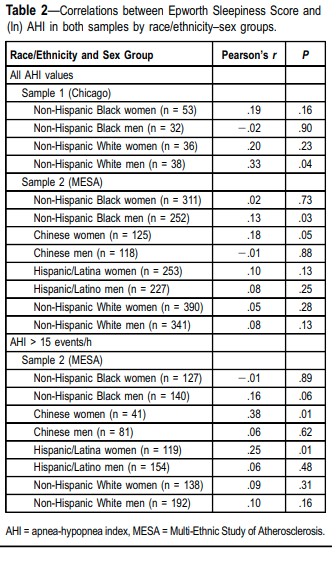
A positive effect of dronabinol on AHI was already known from the literature, but the combination with atomoxetine had not been tested to date. Several mechanisms may modulate the drop in AHI (Figure 2), ODI, hypoxic burden, and cT90 observed on Ato-Dro (Table 2). Atomoxetine has been shown to have a direct stimulant effect on the pharyngeal muscles and dronabinol could have similar synergistic properties The plausible activity of atomoxetine and dronabinol on the upper airway muscle is reflected by the changes in VACTIVE, which was increased on atomoxetine alone and further increased on Ato-Dro 80–5 mg vs. baseline (Table 4). Notably, a higher VMIN might also mirror improved collapsibility due to upper airway muscle stimulation and less frequent dips in ventilatory drive (an important pathogenic mechanism in OSA). Dronabinol-driven sleep stabilization could also play a role in improving upper airway patency via preventing atomoxetine-related sleep disruption,an action that was previously attributed to oxybutynin when combined to atomoxetine. Despite no change in arousal threshold being observed across the nights, several findings potentially support the hypothetical hypnotic properties of dronabinol, such as (1) the reduced self-reported sleepiness and fatigue (per PROMIS questionnaires) on Ato-Dro vs. baseline and vs. atomoxetine alone, (2) the increase in non-REM stage 2 sleep on Ato-Dro vs. baseline, and (3) the improvements in total sleep time and wake after sleep onset on Ato-Dro 80–10 mg vs. atomoxetine alone (Table 2). Indeed, the effect on total sleep time seen with Ato-Dro, occurring despite the absence of arousal threshold improvements, is consistent with what has been observed with other sedatives. However, given the design of this study, these findings should be interpreted with caution. Of note, breathing stabilization (via dronabinol-mediated inhibition of no dose ganglion 5-hydroxytryptamine receptor 3 (5-HT3)) did not seem to have a role in decreasing OSA severity while on Ato-Dro, as loop gain was overall unchanged across all study nights (Table 4).



Comments